With no drug yet proven to reduce deaths due to COVID-19, scores of clinical trials are underway testing already available drugs (marketed and investigational) in the hope that one or a combination of these will be effective. Unfortunately, outside of these trials, many patients are being treated with drugs that have potentially lethal side effects which raises the very important question…. Are these drugs saving more lives than they might be taking? The drug labels for three of these drugs, hydroxychloroquine (HCQ), chloroquine (CQ) and azithromycin, include stark warnings for the rare but real possibility of death due to their effects on the heart. Among other cardiac risks, they each prolong the electrocardiographic QT interval which predisposes patients to sudden arrhythmic death. Their drug labels also warn that combining them with other QT prolonging drugs increases the danger. However, detecting such harm in clinical trials is not simple. Rare adverse events such as drug-induced deaths are impossible to quantify without data from large numbers of treated patients and the ability to compare their outcome to that in an untreated group that is balanced for the many confounding factors that can bias outcomes. Without blinded randomization to a treated group or placebo, a balanced comparison is difficult to make because of doctors’ natural tendency to treat the sickest patients with drugs that they think may have any chance of efficacy.
We now have two studies that help us address the question posed above, i.e. Do these drugs save lives? The first study, published May 22nd in the Lancet , had the sample size needed to detect rare events such as drug-induced death. The authors collected data from over 96,000 very ill hospitalized patients and concluded that both HCQ and CQ, alone or combined with azithromycin, did not improve mortality and that deaths and ventricular arrhythmias were 35% higher in the treated patients. The second study was smaller but, in this case, the investigators randomized the patients to receive two different doses of CQ. The frequency of death was 39% (16/41) in the higher dose group and 15% (6/40) in the lower dose group. Based on these results, most would agree that there is no scientific or ethical justification for further treatment or testing of these drugs in very ill patients because they do not reduce overall deaths and more likely take more lives than they save.
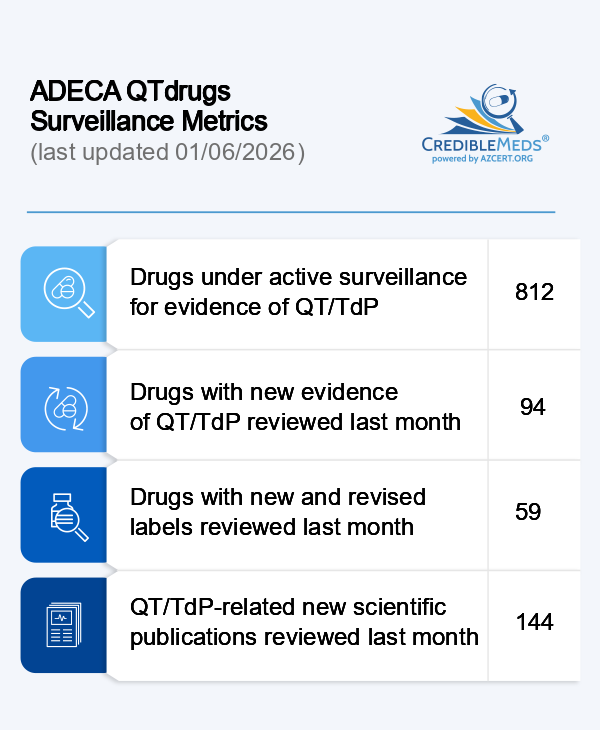
Randomized prevention trials remain underway to test HCQ in healthier, uninfected patients and most include careful ECG screening and monitoring for QT prolongation. These trials can still be justified because of the assumption that the risk of serious drug-induced events such as arrhythmic death is likely to be lower than that in the very ill hospitalized patients enrolled in prior trials. Importantly, most trials screen participants to exclude anyone who is more likely to be harmed, such as those with congenital long QT syndrome or those taking any of the 180 drugs known to prolong QT. On April 27, AZCERT launched a website (www.medsafetyscan.org) for a computerized decision support program to assist clinical researchers and other healthcare providers screen and monitor patients in clinical trials. MedSafety Scan was developed by AZCERT in collaboration with the FDA’s Safe Use of Medicines program. We encourage everyone testing drugs for COVID-19 to utilize this open source resource.